by Maxine Lipner EyeWorld Senior Contributing Writer
Considering topography-guided PRK treatment
Ophthalmologists must content with corneal scars resulting from ulcers and ocular trauma. Study results in an investigation led by Nir Sorkin, MD, cornea fellow, University of Toronto, which appeared in the Journal of Refractive Surgery, indicate that topography-guided PRK may be a valuable treatment tool here.1
There is a lot of variety in what causes a scar. “Corneal scars affect vision due to opacification of the cornea, stromal remodeling, which affects corneal optics, or by creating an irregular corneal refracting surface, which induces irregular astigmatism,” Dr. Sorkin said, adding that all of those can affect uncorrected and best corrected visual acuity.
Investigators were spurred to consider the topography-guided PRK approach by the fact that available treatment options fell short in one respect or another. Offering patients rigid gas permeable or scleral contact lenses, for example, addresses surface irregularity but does not affect the stromal changes, which constitute the scar, Dr. Sorkin noted. Other treatment options also have limitations. “Superficial keratectomy, PTK, and PRK aim to debulk the scar while also regularizing the surface,” Dr. Sorkin said. “However, they are not customized to the irregularity of the specific cornea that is being treated.” This might limit their effect on corneal irregularity. Keratoplasty removes the corneal scar altogether but is a more complex procedure that could also result in significant postoperative astigmatism, Dr. Sorkin said.
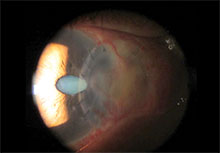
One of the study cases where topography-guided PRK was used to treat high and irregular corneal astigmatism due to nasal corneal scarring. Scarring occurred following a nasal corneal perforation that required lamellar keratoplasties. Source: Nir Sorkin, MD
Topography-guided PRK
The idea was to see whether topography-guided PRK could provide a more comprehensive approach here. “Topography-guided PRK has all the advantages of standard PRK, with the addition of a laser ablation algorithm that is guided by the specific topography of the cornea that is being treated,” Dr. Sorkin said. “This modality is being used to treat irregular astigmatism caused by other pathologies such as keratoconus and refractive surgery complications and also to treat irregular astigmatism following keratoplasty.” With this in mind, investigators thought topography-guided PRK could be a good choice in the treatment of corneal scarring.
Included in this retrospective case series were six eyes of six patients who had corneal scarring with corneal surface irregularity with reduced best corrected and uncorrected visual acuity. “In some cases, the procedure was performed to try and improve visual acuity enough to eliminate the need for a corneal transplant,” Dr. Sorkin said. “In other cases, where cataract was also present, topography-guided PRK was performed to regularize astigmatism in a way that could enable implantation of a toric IOL.” Patients included here underwent one topography-guided PRK procedure and in some cases subsequent enhancement procedures, he explained, adding that these were either topography-guided PRK in cases where residual irregular astigmatism was present or standard PRK in cases where the cornea was regular enough but a substantial refractive error was present.
Investigators determined that results were promising. “The topography-guided PRK procedure did improve uncorrected and best corrected visual acuity in some of the patients to a level that they did not require further intervention,” Dr. Sorkin said, adding that it also obviated the need for a corneal transplant in others. In cases where the treatment was paired with cataract removal, use of topography-guided PRK regularized corneal astigmatism, making it possible to implant a toric IOL.
Embracing the procedure
There were no intraoperative or postoperative complications in these cases, Dr. Sorkin stressed. However, recovery did take some time. This is something that practitioners should keep in mind when offering the procedure clinically. “Patients should be properly counseled that visual recovery following topography-guided PRK performed on irregular corneas might be a long process with stabilization of corneal changes and refractive error occurring up to 6 months after surgery, and possibly even longer,” Dr. Sorkin said. “Also, they should be informed that additional refractive procedures might be necessary to further regularize the cornea or address refractive error that remains or that is induced by the treatment.”
In some cases, topography-guided PRK might induce an increase in the refractive error that could reduce patients’ uncorrected visual acuity, making them initially think that their vision is worse, despite the fact that there is an improvement in their best corrected visual acuity.
It is incumbent on practitioners to ensure that the residual stromal bed is thick enough to allow for multiple procedures, Dr. Sorkin stressed. “It is also crucial to obtain high quality and consistent topography scans that would guide precise treatment algorithms,” he said. Practitioners should avoid selecting those with severely irregular corneas. They also usually limit the difference between the steepest and the flattest areas of the irregular cornea to 10 D.
When evaluating a patient, Dr. Sorkin advised practitioners to offer a trial of a rigid gas permeable or scleral contact lens, which could simulate the effect of corneal regularization to see the potential for improvement with topography- guided PRK. “We use this method as a preoperative simulation, and in cases where this trial does not cause any improvement, we reconsider the treatment,”
Dr. Sorkin said. “It is also recommended to use anterior segment OCT to evaluate the depth of the scar, as deeper scars might not benefit from the treatment.” Dr. Sorkin hopes practitioners come away from the study with the realization that this is a potentially valuable addition to the armamentarium. “Topography-guided PRK is another good tool that can help the management of corneal scarring,” he said. “However, proper case selection and patient counseling are crucial.” Dr. Sorkin views the approach as one that will continue to emerge. “Topography-guided PRK should be considered as an option in cases of corneal scarring, and potentially even more so in the future as customized treatment algorithms continue to evolve,” he said.
Reference 1. Sorkin N, et al. Topography-guided photorefractive keratectomy in the treatment of corneal scarring.
J Refract Surg. 2017;33:639–644.
Editors’ note: Dr. Sorkin has no financial interests related to his comments.
Contact information Sorkin: nir.sorkin@gmail.com
Source: https://www.eyeworld.org/